When 1 in 5 Americans have a sexually transmitted infection, do you know when and where to get tested?
Words & Photography by Taylor Heckart
Ky Martin is in the middle of doing his weekly condom deliveries. On Wednesdays, he goes to universities, bars, rec centers, bookstores, and anywhere that will welcome him. He gets to talk about his job, connect with new organizations, and pass out safer sex materials. It’s one of the best parts of his week.
Right now, he’s got about 18 different places across the Anchorage Bowl that he distributes to on varying schedules.
Martin is the HIV prevention coordinator for the Anchorage Health Department. He tries to offer a variety of condoms to his stops, latex-free, different sizes (it’s a common misconception, he says, that condoms are one-size-fits-all), even offering dental dams—anything to give people options for safer sex.

There’s only one stipulation for Martin’s condom deliveries—if you take them, you have to distribute the condoms for free.
“If I give you condoms, you cannot charge for them. If you do, I take them back,” Martin said.
Delivering condoms isn’t just about preventing pregnancy– it’s also the only form of contraception that prevents sexually transmitted infections.
Alaska is no stranger to STIs. According to the CDC, by 2022 Alaska was ranked third highest in the nation per capita for chlamydia and fourth-highest for gonorrhea.
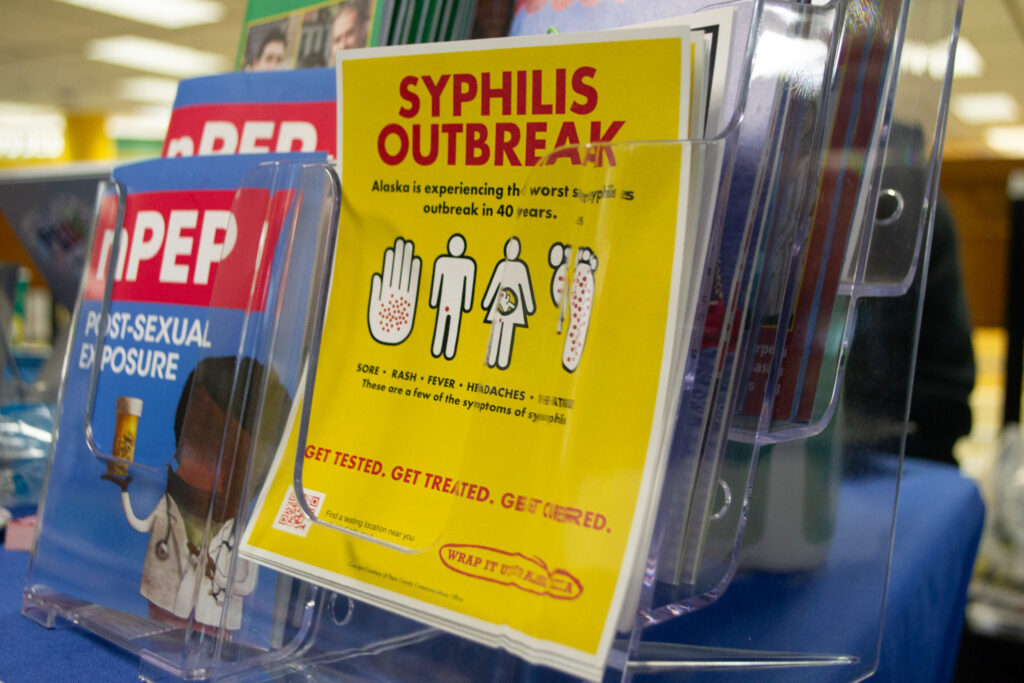
Right now, Alaska’s syphilis cases are also increasing, and it’s a point of concern for many organizations.
In January of this year, the Alaska Department of Health put out a press release advising that most adults under the age of 45 be tested for syphilis at least once in 2024.
Syphilis cases have grown dramatically in recent years. Within six years, Alaska’s syphilis cases jumped from 20 cases in 2016 to 424 in 2022–a more than 25-times increase.
This increase follows national trends. According to the CDC, syphilis cases have grown by 80% nationwide in the past five years.
Condoms aren’t the only resources in the fight against STIs. The sexual health resources and treatment provided by the Anchorage Health Department and other local organizations are vital in combating increasingly high rates of STIs across the state. In some cases, these resources are lifesaving.
The Symptoms and Risks Of Syphilis
Liz Ohlsen is a staff physician in the section of epidemiology with the Division of Public Health for the State of Alaska. She’s also the acting program manager for the HIV and STD program.
She said that with syphilis, symptoms can be “subtle.”
“When they first get infected, they may see a sore or an ulcer. A lot of times it’s not painful, a lot of times it’s in somewhere that’s hard to see or can be mistaken for other things […]. So sometimes people may not notice anything at all,” said Ohlsen.
Since symptoms can be hard to spot, it can be easy to think that nothing is wrong. Another aspect of syphilis that makes it hard to identify is “that sore tends to go away for a while. So it may last a few days to a few weeks, and then it goes away on its own. And it doesn’t mean the infection has gone away. In fact, that person remains infectious.”
According to the CDC, after the first stage of syphilis, people may experience a rash on different parts of their body. Other symptoms may include a fever, headaches, weight loss, or fatigue. These symptoms may also go away on their own.

Ohlsen said that it’s easy to mistake these symptoms for another illness or infection.
“I think there’s a real possibility of having, kind of like a false sense of security or […] a certainty that this might have been something else. But unfortunately, that person will continue to have syphilis infection until they’re treated, and they may still be infectious for a while after that.”
Without treatment, there is also a chance that syphilis can spread to the brain and nervous system at any point. For individuals who have had syphilis in their bodies for longer than 10 years, the CDC says there is also a chance of developing tertiary syphilis, which attacks internal organs and can lead to death.
Rising syphilis rates have also led to higher rates of congenital syphilis, which happens during pregnancy when syphilis is passed from a pregnant person to their baby. The effects of congenital syphilis can be devastating, sometimes leading to miscarriages, stillbirths, or birth deformities.
Since syphilis can be easily mistaken for other illnesses–but can be damaging if left untreated–syphilis testing and contact tracing are vital.
Ohlsen’s team works to connect individuals with STI resources and treatment across the state. They also anonymously and confidentially contact partners of someone who has tested positive for syphilis, and inform them that they should be tested as well.
The good news is that congenital syphilis is entirely preventable, and syphilis is absolutely curable. For most people, Ohlsen said, it’s often as simple as getting a shot of penicillin– though treatment may be more involved if syphilis has been in the body for long periods of time.
Drastic Growth and Low Awareness
With syphilis numbers rising, how much do Alaskans know about syphilis? That was the question that some students in Dr.Angelia Trujillo’s Nursing Care of Communities and Populations class set out to answer in the fall of last year.
This class is a course that nursing students take in their final year at UAA, and students spend time researching, speaking to individuals with key knowledge, creating surveys, and then analyzing data and coming up with recommendations around various health topics.
Trujillo calls the class, “work beyond the bedside,” as it helps nursing students make connections between hospital nursing and public health issues.
Two groups in the course focused on syphilis: one on syphilis in adults and the other on congenital syphilis.
Both groups surveyed more than 200 people.Their data can be found in the Health Sciences Building at UAA.
Surveys found that while most people had heard of syphilis, many didn’t know how it was spread. Similarly, in the case of congenital syphilis, a majority of respondents were either completely unaware or only somewhat aware of the risks of passing syphilis to a baby during pregnancy.
These surveys were completed before the state’s press release on syphilis, but Trujillo said that it was easy to see the syphilis spike coming.
“In the case of syphilis, you know, in a state the population size that we have, you know, two or three cases is already an epidemic, right?” said Trujillo.
“So much of the infectious process is silent. And so we have been seeing just a … steeply rising increase over the past three or four years.”
Trujillo said that this course allows students to understand that STIs don’t just happen to one group of people. Trujillo said it’s a common misconception that syphilis is only an issue for populations of men having sex with other men. Syphilis, however, is also being found in heterosexual couples, women, and children.
It does not matter what your gender, sexuality, or socioeconomic status is; anyone can get syphilis.
Walk-In STI Testing, All For Free
Sometimes the cost of an STI test can be a barrier to receiving health care, but some organizations frequently offer free testing services.
The Anchorage Health Department offers free walk-in STI testing on Mondays and Fridays to anyone over the age of 13. They offer screenings for HIV, gonorrhea, chlamydia, and syphilis.
Martin, with the Anchorage Health Department, said that the clinic has definitely been seeing higher rates of syphilis. They’ve also seen the use of the walk-in clinic grow after the clinic reopened post-pandemic.
“When we started it back up […] first it was like two or three people, and then it started going to five to six people and continuing. We see about thirty people in a day,” Martin said.
There’s no such thing as a one-size-fits-all STI test–testing can vary depending on what STIs you’re looking for and how you’re having sex. Blood tests, swab tests, and urine tests are all common ways to receive STI tests.

Martin said that if someone tests positive for an STI they do same-day treatment if they can. If not, they’ll have a follow-up appointment or send a prescription to the pharmacy to pick up.
Martin said that free or sliding-scale clinics–like the one the municipality operates–are important because they give people knowledge about their status.
Resources Mailed Statewide
There are also programs providing STI resources for those outside of Anchorage.
iKnowMine is a program by the Alaska Native Tribal Health Consortium that provides a wide variety of health resources for Alaska Native and rural Alaskan youth.
Hannah Gumlickpuk is an HIV/STI program manager with the Alaska Native Tribal Health Consortium and said that IKnowMine started in 2009 to address the high rates of gonorrhea and chlamydia in Alaska. The program eventually expanded to become a holistic website centered around youth.
Though IKnowMine’s resources often prioritize Alaska Natives, anyone in the state can use and order these materials.
Among those resources, IKnowMine also offers an online “shop” that offers free condoms and dental dams. They’ve also partnered with I Want The Kit, an initiative of Johns Hopkins University School of Medicine, to provide free HIV and STI test kits. The kits are meant to be easy to do at home, and come in confidential packaging.
These test kits are a vital way to reach people in communities where there are less options for care.
“I do think, you know, being able to serve our rural communities and being able to work with our partners to reach folks where they’re at, I think that’s definitely work that we excel at,” Gumlickpuk said.
A report from the Alaska Native Tribal Health Consortium reported that during 2020, Alaska Native/American Indian people experienced chlamydia at a rate 3.8 times higher than non-native people, and gonorrhea at a rate 3.9 times higher. The factors behind those higher rates are complicated.
“I think we do a really good job of testing communities, I think that may contribute to the higher rates as well,” said Lisa Rea, a Nurse Case Manager at the Alaska Native Tribal Health Consortium.
“I also think, you know, access to like, prevention supplies and tools in many rural communities is a little bit more challenging as well,” said Gumlickpuk.
“But then also, I think it also comes down to, you know, Alaska Native people are able to connect with the local tribal health organizations. And you know, in a lot of instances, you know, that the testing is at no cost. And that’s not something that a lot of people are able to access as often as well.”
Uneven Education In Schools
If you ask Madeline Cooper why STI rates are so high in Alaska, Cooper would say that education is a massive component. Alaska has no mandated sexual education requirement, so the extent to which students receive sex education can vary.
Cooper is the community outreach educator working with Planned Parenthood. She works with high school students who are a part of Planned Parenthood’s Teen Council, a peer-led program where 10th-12th graders teach other students about sex and reproductive choices. In February, Teen Council was teaching classes at Highland Academy–though all attendees had to have parental approval in advance.
In February, as a part of Planned Parenthood’s Teen Lobby Day, they went to Juneau to advocate for mandatory comprehensive sex education.
“We want them to know these teens’ stories and hear the impact that legislation like this has on youth today,” Cooper said.
One part of comprehensive sex education? Providing information for LGBTQ+ youth.
“Young, gay and bisexual youth have disproportionately high rates of HIV, syphilis and other STIs and adolescent lesbian and bisexual women are more likely to have been pregnant than their heterosexual peers,” said Cooper.
According to the World Health Organization, evidence shows that comprehensive sexual education leads to young people waiting to have sex, reduces risky behaviors, and leads to increased use of contraceptives.
Peer-to-Peer Conversations
At UAA, another peer-to-peer program is bringing health education to college students– the Peer Health Education Team. Students on the team talk about a wide variety of health topics, from mental health to healthy relationships. They also talk about sex education.
The team is behind UAA’s condom dispensers, which can be found in bathrooms and spaces on campus. They get condoms for free from multiple organizations, including the Anchorage Health Department and iKnowMine. The team also hosts health fairs and free STI testing events at UAA.

Summer Sweet, the health promotion specialist for the team, said that sometimes it can be awkward for students to talk about such stigmatized topics with their team.
Sweet said oftentimes a lack of sexual education can make students hesitant to talk to their team. “We’re just trying to reduce the stigma to and like make it a very common thing for people to be able to talk about.”
Fabiola Lugo-Vazquez, the health educator assistant with the Peer Health Educators, said that after talking to their team, students often “have a really good attitude toward the end” and get excited about their work.
So, What Do I Do To Avoid STIs?
The only way to 100% prevent receiving syphilis, or any other STI is to abstain from having sex.
For those who choose to be sexually active, it’s important to know both your status and any partner’s status. Many STIs are asymptomatic, so being proactive and testing every time you are with a new partner is a good idea. For individuals who have sex with multiple or anonymous partners, it’s a good idea to get tested every 3 – 6 months.
Ohlsen, with the Department of Health, said that talking about your STI status can be a part of broader conversations that you have with your partner about health.
Regularly using barrier protection such as condoms or dental dams can also help reduce your risk of receiving an STI. Other forms of birth control that protect against pregnancy, such as the pill or the implant, do not protect against STIs– only barrier protection can do that.
And, if you are infected with an STI, there are resources and treatments out there for you.
“All STDs are treatable, most are curable.”
True North is a publication of the University of Alaska Anchorage Department of Journalism and Public Communications. It has been published since 1995.

